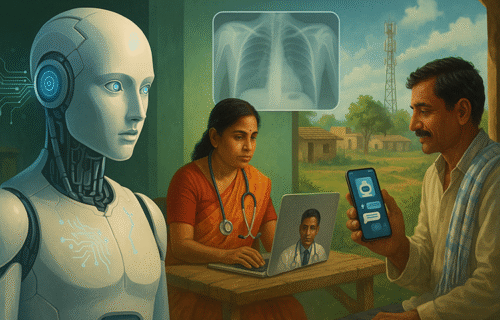
Artificial intelligence is moving from pilot projects to frontline care across India, with its biggest promise showing up far from tertiary hospitals. Telemedicine, AI-assisted diagnostics and multilingual chatbots are beginning to narrow long-standing access gaps for villages and tribal communities that struggle to attract specialists.
India’s state-run eSanjeevani platform illustrates the scale of the shift. Government figures show it surpassed 360 million teleconsultations by April 2025, making it one of the world’s largest national telemedicine services. Academic reviews describe it as a crucial “hub-and-spoke” network linking primary facilities to district and specialist hubs, particularly valuable in rural areas.
Diagnostics are where AI’s leverage is most visible. Computer-aided detection software for chest X-rays—now recommended by the World Health Organization for triage and screening—has been evaluated in India and other high-burden settings and can flag likely tuberculosis cases when radiologists are scarce, speeding referrals for confirmatory testing. Several Indian deployments, including projects assessed by PATH and others, report gains in TB case-finding and potential cost savings. Tamil Nadu’s health department is the latest to expand pilots of AI-assisted imaging for TB and other conditions in government hospitals, with the stated goal of supporting clinicians rather than replacing them.
AI is also feeding into disease surveillance and public-health preparedness. Indian researchers have built early-warning models that fuse climate and health data to predict dengue outbreaks weeks in advance, giving local authorities lead time to target vector control. State and municipal bodies are testing complementary digital tools—from smart mosquito-monitoring sensors to drone-enabled fogging—to contain vector-borne disease risks during monsoon seasons.
The rural frontline is benefiting from language-aware tools that match India’s linguistic diversity. The government’s Bhashini initiative is building translation and speech APIs so citizens and health workers can access services in local languages. In parallel, research programmes have released health chatbots tailored to community health workers, such as Microsoft-backed ASHABot and the George Institute’s SMARThealth GPT, which surface official guidance in Hindi, Telugu and other languages and allow voice interactions in low-resource settings.
Connectivity remains the critical enabler. India’s 5G rollout has accelerated since late 2022; by March 2025 the government reported 469,000 5G base stations with services in nearly every district, although independent analyses still point to uneven backhaul and variable latency outside major corridors. For remote teleconsultations and AI tools that rely on real-time image transfer, these bottlenecks can be the difference between a same-day diagnosis and a referral that never happens.
Claims that AI has already solved rural healthcare are premature, and several cautions are warranted. Researchers reviewing eSanjeevani’s operations flag inconsistent training for frontline staff, gaps in feedback loops and the need to better integrate general practitioners so referrals do not stall. Data governance and privacy protections have to keep pace as more imaging and clinical metadata move through cloud systems. And as generative AI lowers the cost of producing persuasive content, public-health agencies are confronting a parallel challenge: disinformation during outbreaks or tense civic moments that can overwhelm credible guidance.
Even so, the direction of travel is clear. A mix of high-volume telemedicine, AI-assisted diagnostics and locally intelligible digital tools is pushing specialist expertise closer to the village clinic. The policy task now is to lock in the basics—reliable connectivity, workforce training and procurement pathways that privilege clinically validated AI—so early gains in access turn into durable improvements in rural health outcomes.
© 2025 www.cijeurope.com